
A healthy vagus nerve supports your digestive system, helps to regulates your sleep patterns, and calms down your nerves. Learning to regulate vagal tone is associated with a reduction in inflammation and better prognosis in people suffering from chronic illness, migraines, auto-immune disorders, anxiety, and depression. If you suffer from any of these vagus nerve disorders, then this post is for you.
“Healthy vagal tone involves engaging your social nervous system. You can learn to manage the symptoms of vagus nerve disorders by skillfully working with your mind and body to tone your vagus nerve. Mind-body therapies effectively increase your resilience by helping you develop your capacity to feel safe, calm, and connected—even during times of stress.”
-Dr. Arielle Schwartz
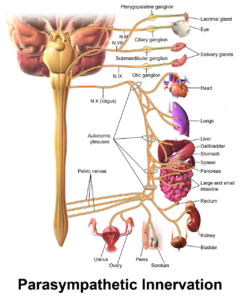
Research by Dr. Stephen Porges explores the connections between early attachment history, traumatic exposure, and your health as related to the functioning of the vagus nerve (the tenth cranial nerve). The vagus nerve connects the brain to major systems in the body including the stomach, gut, heart, lungs, throat, and facial muscles. Porges’ Polyvagal Theory (PVT) proposes that there are three functions of the autonomic nervous system: social communication, defensive mobilization, and defensive immobilization. (You can read more about polyvagal theory and PTSD here.) Getting stuck in defenses responses is a key contributor to vagus nerve disorders.
The social communication system, also known as the “ventral vagal complex” (VVC) is the branch of the vagus nerve which has a calming and soothing effect. Your social nervous system gets its name because it is responsible for your facial expressivity. In addition, the social nervous system is responsible for both the expressive and receptive domains of verbal communication. This guides the rhythm and tone of your speech and helps provide meaning to your communications. Furthermore, your social nervous system enhances your ability to listen to others allowing you to pick up on emotional nuances within communications. And, considering that the vagus nerve links the heart to the muscles of your face, you will be more likely to engage empathic responses.
Vagal tone is measured through the oscillations in heart rate variability that occur with the breath. This is referred to as Heart Rate Variability or HRV. Healthy tone of your vagus nerve involves a slight increase in heart rate on the inhalation and a decrease inheart rate when you exhale. According to Bessel van der Kolk (2006), “Heart rate variability (HRV) provides the best available means of measuring the interaction of sympathetic and parasympathetic tone, that is, of brainstem regulatory integrity.”
Healthy vagal tone can be thought of as an optimal balance of parasympathetic and sympathetic nervous system actions. People with higher HRV can move more easily from excitement to relaxed and can recover more easily from stress.
Individuals with long-term, chronic trauma exposure can lose the ability to accurately perceive whether people or places are safe or trustworthy.
In other words, you might respond to a situation as threatening when you are actually safe. In these situations, you can learn to override unnecessary defensive traumatic reactions of fight, flight, freeze, or faint.
Engaging your social nervous system helps to manage vagus nerve disorders. Your social nervous system is strengthened by repeated practice which myelinates the nerve pathways. Myelination is the fattycoating on nerves that is developed through repeated use and leads toincreased speed and control.
Once you know how to engage your social nervous system you can apply these skills during times when you feel keyed up with anxiety or contracted into depression. Engagement of your social nervous system while mobilized by your sympathetic nervous system allows you to access your creativity, become playful, and dance with the available energy.
Conversely, engaging your social nervous system when you feel shut down by traumatic memories might allow you to override unwarranted defensive immobilizing reactions. Here you can focus on connecting with your heart in a place of stillness or connecting with a loved one for greater intimacy. Such a blend is also valuable to facilitate ease during childbirth, nursing, or bonding. Porges (2017) suggests that this blend can assist you to connect to a universal unbounded sense of oneness.
Mind-body therapies regulate the vagus nerve and increase your resilience through “safe mobilization and safe immobilization” (Sullivan et al., 2018). This involves initially developing your capacity to feel peaceful, calm, and connected. Once you have a solid foundation of being able to access your social nervous system you can slowly build your tolerance for distressing physiological activation. This is accomplished by blending social engagement with both mobilization and immobilization until you can re-establish a sense of safety with those nervous system states. Over time, you increase your capacity to move in and out of different nervous system states.
Mind-body therapies and somatic psychology invite you to simultaneously attend to your body sensations, breath, emotional experience, and your thoughts. Additionally, you focus on sensing your external environment which will help you recognize that you are safe here and now. Some practices involve mindful use of movement (e.g. yoga postures, tai chi, walking meditation) and others, mindful use of stillness (seated meditation, relaxation, yoga nidra).
Engaging the vagus nerve during movement or stillness can allow for different social nervous system blending for varying health needs and energy levels. Explore the following 4-Part practice designed to help you recover from vagus nerve disorders:
Begin by finding a place where you know you are safe to explore this mind-body practice. Find a comfortable position either standing, seated, or laying down. Look around your space, identify visual cues that tell yourself that you are safe, here and now. Repeat to yourself these words throughout the practice, “I am safe, I am connected, I am calm.”
Take several long, deep breaths. Notice the sensations of the breath in your body and the subtle movements created by your breath. Now, bring your awareness to the sound of your breath. Expand your sensory awareness to notice any other sensations in your body. Repeat the phrase, “I am safe, I am connected, I am calm.” If at any point in the practice you experience anxiety or other distress return to step one by looking around your space to remind yourself that you are safe now.
Now, begin to explore increasing the intensity of your breath while moving your body. Maybe you stand up into an active yoga posture. Perhaps you walk vigorously in place or around the room. You can even put on your favorite song and dance! Increase your heartrate just enough to notice that your breath quickens to support your movement. Repeat your phrase, “I am safe, I am connected, I am calm” as you move your body. Once again, if you experience any anxiety or other distress, look around your space to remind yourself that you are safe now.
The final step of this practice invites you to return to stillness either standing, seated, or laying down. Allow your heartrate to slow down. Surrender your weight down toward the earth. Invite long, deep breaths extending your exhale longer than your inhale to initiate a relaxation response. Choose to be still and soften any unnecessary holding in your muscles. Repeat your phrase, “I am safe, I am connected, I am calm” as you connect to stillness. Once again, if you experience any anxiety or other distress, look around your space to remind yourself that you are safe now.
References:
Within The Post Traumatic Growth Guidebook, you will find an invitation to see yourself as the hero or heroine of your own life journey. A hero’s journey involves walking into the darkness on a quest for wholeness. This interactive format calls for journaling and self-reflection, with practices that guide you beyond the pain of your past and help you discover a sense of meaning and purpose in your life. Successful navigation of a hero’s journey provides opportunities to discover that you are more powerful than you had previously realized. Click here to order the book on Amazon.
As a compliment to the Complex PTSD Workbook, A Practical Guide to Complex PTSD: Compassionate Strategies for Childhood Trauma, is meant to provide compassionate support for the process of healing from childhood trauma. You can think of it as a lantern that will illuminate the dark spaces and provide a sense of hope in moments of despair. The practical strategies you will learn in this book are taken from the most effective therapeutic interventions for trauma recovery. You will learn the skills to improve your physical and mental health by attending to the painful wounds from your past without feeling flooded with overwhelming emotion. My wish is to help you discover a new sense of freedom. The traumatic events of your past no longer need to interfere with your ability to live a meaningful and satisfying life. Click here to Order on Amazon.
In The Complex PTSD Workbook, you’ll learn all about Complex PTSD Recovery and gain valuable insight into the types of symptoms associated with unresolved childhood trauma, while applying a strength-based perspective to integrate positive beliefs and behaviors. This is a great add-on with the Post Traumatic Growth Guidebook…Click here to order.
For therapists, The EMDR Therapy and Somatic Psychology book, teaches you how to integrate two of the best known trauma recovery modalities into your practice. Click to order it here and increase your toolbox for healing using this integrative and effective approach to healing.
Dr. Arielle Schwartz is a licensed clinical psychologist, wife, and mother in Boulder, CO. She offers trainings for therapists, maintains a private practice, and has passions for the outdoors, yoga, and writing. She is the developer of Resilience-Informed Therapy which applies research on trauma recovery to form a strength-based, trauma treatment model that includes Eye Movement Desensitization and Reprocessing (EMDR), somatic (body-centered) psychology and time-tested relational psychotherapy. Like Dr. Arielle Schwartz on Facebook,follow her on Linkedin and sign up for email updates to stay up to date with all her posts. Dr. Schwartz is the author of four books:

Arielle Schwartz, PhD, is a psychologist, internationally sought-out teacher, yoga instructor, and leading voice in the healing of PTSD and complex trauma. She is the author of five books, including The Complex PTSD Workbook, EMDR Therapy and Somatic Psychology, and The Post Traumatic Growth Guidebook.
Dr. Schwartz is an accomplished teacher who guides therapists in the application of EMDR, somatic psychology, parts work therapy, and mindfulness-based interventions for the treatment of trauma and complex PTSD. She guides you through a personal journey of healing in her Sounds True audio program, Trauma Recovery.
She has a depth of understanding, passion, kindness, compassion, joy, and a succinct way of speaking about very complex topics. She is the founder of the Center for Resilience Informed Therapy in Boulder, Colorado where she maintains a private practice providing psychotherapy, supervision, and consultation. Dr. Schwartz believes that that the journey of trauma recovery is an awakening of the spiritual heart.