Many distressing symptoms of post-traumatic stress are felt in the body—a tightness in the chest, a sinking feeling in the stomach, a familiar knot in the throat, or as a chronic feeling of exhaustion. We now recognize that we must turn toward the body as part of the healing process and as a result we have seen a surge in the use of yoga, mindfulness, tai chi, Qigong, Feldinkreis, massage, craniosacral, nutritional counseling, and acupuncture for the treatment post traumatic stress.
These mind-body therapies help us to be less vulnerable to stress, less reactive, and less impulsive. We increase our awareness of the choices that we have to help us feel grounded and calm. We feel more in control. One way that mind-body therapies work is by stimulating the vagus nerve. Knowledge about how this nerve works provides a fundamental understanding of traumatic stress and facilitates our ability to heal. As a result, the vagus nerve has taken central stage in trauma treatment.
“Mind-body therapies work with the vagus nerve to help you find balance. In this post, you will find a variety of breath and movement practices aimed to stimulate and reset the vagus nerve. Through a process of self-study and mindful body awareness, you can start to learn strategies that help you restore a sense of safety and heal from trauma.”
-Dr. Arielle Schwartz

The use of mind-body therapies is associated with a wide range of changes[1]in health and wellbeing including:
Several mechanisms help explain how mind-body therapies lead to relief from symptoms. They help us reflect upon our thoughts, emotions, and motivations for behaviors. This capacity to observe helps to increase distress tolerance and can lead to decreased emotional reactivity, anxiety, panic, chronic pain, and depression[2]. Furthermore, mind-body therapies enhance self-compassion and the ability to compassionately view another person’s point of view.
In addition, mind-body therapies are effective because they engage physiological changes in the autonomic nervous system as measured by changes in the functioning of the vagus nerve. The vagus nerve extends from the brainstem down into the muscles of the face, inner ear, throat, heart, lungs, stomach, and intestines. Mind-body therapies create changes in how we orient to our environment by inviting a soft gaze and invite us to explore new patterns of breath or movement that directly interact with these areas of the body. One of the ways that researchers measure the changes that happen in the vagus nerve is through heart rate variability (HRV)[3] also referred to as respiratory sinus arrhythmia.
HRV refers to the rhythmic oscillations of your heart rate that occur with the breath. It is a measure of the intervals between your heart beats. Higher heart rate variability is associated with a greater ability to tolerate or recover from stress, whereas lower heart rate variability is associated with stress and anxiety. You can think of any mind-body therapy practice that increases heart rate variability as building flexibility and resilience within your autonomic nervous system. As a result, it becomes easier to move between feelings of excitement and ease.

When we experience a threat (real or perceived), we change how we breathe. Here, we can get a clear picture by imagining the ways in which animals respond to predators. In some cases, an animal will breathe rapidly into the upper chest which is a sympathetic nervous system response that helps them flee from or fight in a threatening situation. In other cases, an animal will freeze which involves breathing shallowly or holding the breath in order to avoid being sensed by a predator. This freeze reaction leads the animal to stand very still which is an immobilization response to threat. In some cases, animals will faint so that a predator who is not a scavenger might lose interest in a dead animal. Both the freeze and faint responses are facilitated by an evolutionarily older pathway of the vagus nerve and part of the parasympathetic nervous system.
Most importantly, once safe, an animal will release the stress response through shaking and breathing in a way that restores homeostasis. However, we humans will often stay in both high activation (fight and flight) or low activation (freeze and faint) responses for extended periods of time. This tends to the be case when trauma is chronic and repeated as in the case of Complex PTSD (you can read more about this here). Additionally, we often do not have sufficient opportunities to process stressful or traumatic events. This can lead to physical tension and restricted breathing patterns that form the basis of our posture, movement patterns, and overall sense of self.

According to Dr. Stephen Porge’s Polyvagal Theory[4], the autonomic nervous system comprises a three-part hierarchical structure: the dorsal vagal system, the sympathetic nervous system, and the ventral vagal system. The dorsal vagal system, which is oldest of the systems, is part of the parasympathetic nervous system. The dorsal vagal nerve immobilizes the body in response to life threatening situations by facilitating a shut down response. The sympathetic nervous system, which is comparatively newer to evolve, mobilizes the body in response to threat by activating the fight-or-flight response. Most importantly, mind-body therapies help to activate the ventral vagal system,which is the newest and most evolved of the structures, This “social engagement” system is the branch of the parasympathetic nervous system that helps you relax and connect to others when you feel safe.
You can learn practices to help reset your vagus nerve; however, not every practice is right for everyone. Instead, I invite you to experiment and explore a variety of breath and movement practices until you find what works for you. Through a process of self-study and mindful body awareness you can start to learn strategies that help you restore a sense of safety and heal from trauma. Here are some resources to help get you started:

You can also increase the health of your vagus nerve by maintaining a healthy digestive system. Theenteric nervous system, also called the belly brain, is made up of the “microbiome” that lives in your gut. This ecosystem contains hundreds of species of good and bacteria that reside within your intestinal tracts. An imbalance in your gut can lead to an inflammatory response in your immune system and cause a wide range of disruptive symptoms, including anxiety and depression. You can create a healthy microbiome by reducing sugar intake and identifying any hidden food intolerances. You may need the assistance of a doctor or nutritionist to discover the causes of a gut imbalance; however, it is well worth the time it makes to integrate these changes into your life.
It has been said that “laughter is the best medicine.” It creates a natural high of endorphins throughout your body. A good belly laugh naturally changes how you breathe, your heart rate, and your blood pressure[5]. Laughter is a body-centered experience; it creates movement in the face, chest, diaphragm, and stomach. So, stay on the lookout for a laughter mediation, a fun friend, or a good comedian to give your vagus nerve a good workout.

Inspired by animals in the wild, you can use a simple shaking practice to let go of physical tension or come out of a freeze response. First, scan your body with your awareness to notice areas of tension. Then, focus on these spots and one at a time give yourself permission to shake them out. Allow yourself to surrender to the shaking and if possible let yourself release any sounds to accompany the movement. When you feel complete, take a moment to pause in the stillness and notice the subsequent release.

Vagus nerve passes by vocal chords and inner ear. Therefore, humming and singing both can have a calming effect on your nervous system. In yoga, Bhamari pranayama, or Honeybee breath provides an opportunity to experiment with a humming sound. In this practice, I invite you to sit in a comfortable position and close your ears with your palms (thumbs facing down). On the exhale create a humming sound to vibrate your eardrum. Repeat as long as desired.

In truth, the vagus nerve is constantly moving us in and out of balance as we are always adapting to the changing demands of our world. Therefore, we often need to repeat vagus nerve balancing exercises. This is the reason why many mind-body therapies are used as a daily practice.
In addition, we need to actually be safe in order to feel safe for these practices to be successful. Sometimes, the cues from our body tell us that we aren’t safe. In this case, we need to honor the message which often requires that we make changes in our lives to protect ourselves.
In contrast, there may also be times that we are reacting to memories of historical traumas in the form of flashbacks. In this case, it may be necessary to work with a therapist who specializes in trauma treatment to heal from the wounds of the past. Otherwise, the “imbalances” in the vagus nerve will likely return until underlying issues are attended to and resolved.
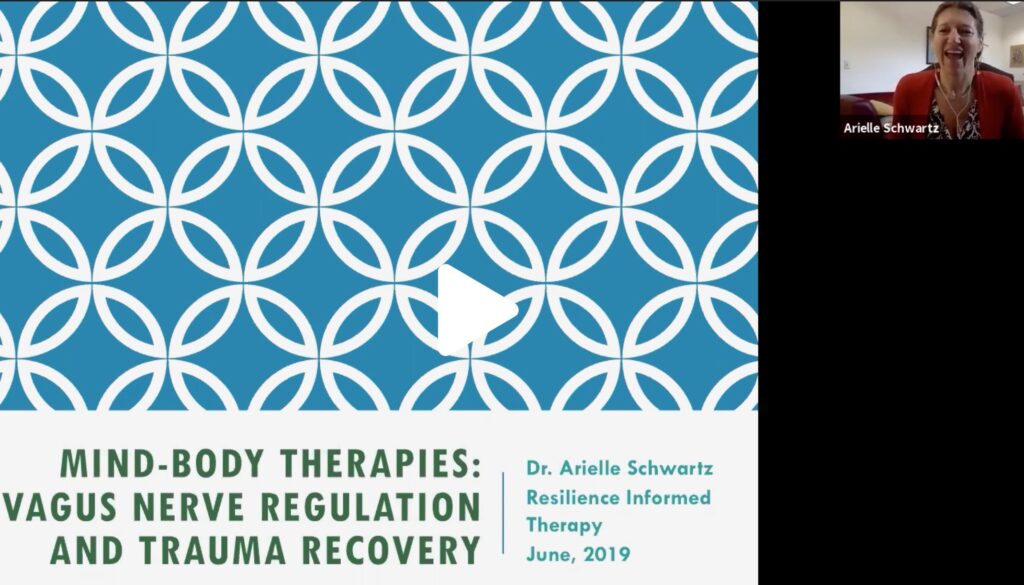
I have created a webinar that is packed with information, resources, and my personal favorite reset strategy for the vagus nerve. Whether you are a psychotherapist seeking to increase your toolbox or are on your own healing journey, you will receive heart-felt guidance and practical strategies for healing. Within this webinar, you will:
Webinar title: Mind-Body Therapies: Vagus Nerve Regulation and Trauma RecoveryPrice: $45

In addition, you can read more about the vagus nerve and trauma recovery here:
References:
[1] Trakroo, M. and Bhavanani, A. B. (2016). Physiological Benefits of Yogic Practices: A brief review. International Journal of Traditional and Complementary Medicine, 1(1), pp. 31-43.
[2] Baer, R. A. (2003). Mindfulness training as a clinical intervention: A conceptual andempirical review. Clinical Psychology: Science and Practice, 10(2), 125-143.
[3] Rosenberg, S. (2017) Accessing the healing power of the Vagus Nerve. Berkely, Ca: North Atlantic Books.
[4] Porges, S. (2011). The polyvagal theory: Neurobiological foundation of emotions, attachment, communication, and self-regulation.New York: Norton.
[5] Dolgoff-Kaspar, R., Baldwin, A., Johnson, M. S., Edling, N., & Sethi, G. K. (2012). Effect of laughter yoga on mood and heart rate variability in patients awaiting organ transplantation: a pilot study. Altern Ther Health Med, 18(5), 61-6.
Image Credits:
The Post Traumatic Growth Guidebook is available now on Amazon. Click here to buy.
Want to learn more about healing PTSD?
Connect to this post? The EMDR Therapy and Somatic Psychology book, is available on Amazon! Click here to increase your toolbox for healing. An integrative and effective approach to healing from trauma.
The Complex PTSD Workbook is available on Amazon! Click here to check it out.

Dr. Arielle Schwartz is a licensed clinical psychologist, wife, and mother in Boulder, CO. She offers trainings for therapists, maintains a private practice, and has passions for the outdoors, yoga, and writing. Dr. Schwartz is the author of The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control and Becoming Whole (Althea press, 2016) and co-author of EMDR Therapy and Somatic Psychology: Interventions to Enhance Embodiment in Trauma Treatment (Norton, 2018). She is the developer of Resilience-Informed Therapy which applies research on trauma recovery to form a strength-based, trauma treatment model that includes Eye Movement Desensitization and Reprocessing (EMDR), somatic (body-centered) psychology and time-tested relational psychotherapy. Like Dr. Arielle Schwartz on Facebook, follow her on Linkedin and sign up for email updates to stay up to date with all her posts.

Arielle Schwartz, PhD, is a psychologist, internationally sought-out teacher, yoga instructor, and leading voice in the healing of PTSD and complex trauma. She is the author of five books, including The Complex PTSD Workbook, EMDR Therapy and Somatic Psychology, and The Post Traumatic Growth Guidebook.
Dr. Schwartz is an accomplished teacher who guides therapists in the application of EMDR, somatic psychology, parts work therapy, and mindfulness-based interventions for the treatment of trauma and complex PTSD. She guides you through a personal journey of healing in her Sounds True audio program, Trauma Recovery.
She has a depth of understanding, passion, kindness, compassion, joy, and a succinct way of speaking about very complex topics. She is the founder of the Center for Resilience Informed Therapy in Boulder, Colorado where she maintains a private practice providing psychotherapy, supervision, and consultation. Dr. Schwartz believes that that the journey of trauma recovery is an awakening of the spiritual heart.