The connections between unresolved trauma and the immune system provide insight into a wide array of medical symptoms. The sympathetic and parasympathetic nervous systems are meant to work in a rhythmic alternation that supports healthy digestion, sleep, and immune system functioning. However, chronic stress and unresolved trauma interfere with the balance between the sympathetic and parasympathetic nervous systems. As a result, unresolved PTSD takes a significant toll on physical health.
“This post takes a closer look at the relationship between stress, trauma, and your health. Developing an understanding of how your body responds chronic PTSD can help you to feel empowered to take a greater role in your health care. When you are informed about your body and mind you attend to challenges of chronic illness with greater success.”
-Dr. Arielle Schwartz
As human beings, we are wired for survival. We will respond with a typical “stress” response whether reacting to an actual or a perceived event. A healthy response to stress involves an increase in cortisols such as adrenaline into your bloodstream that facilitates a fight or flight response in your body. These chemicals give you the energy you need to move and metabolize the energy released in your body. Once there are sufficient levels of cortisols in your bloodstream, your brain receives a signal to stop releasing these neuro-chemicals and you return to baseline. This process is called homeostasis.
Ideally stress is temporary. However, when a stressful situation persists you remain in a state of high alert without the ability to rest. When faced with chronic stress your body will continue to produce high amounts of cortisol. As a result you will likely feel keyed up, jumpy, or anxious.
In contrast, traumatic stress is the result of an event that has life threatening implications. In such a situation fight and flight are unsuccessful. The biological effects of trauma are more enduring and extreme. In the case of unresolved trauma there is a surprising finding–low levels of cortisols within the bloodstream. This does not mean that your body is producing fewer stress chemicals. In fact, you continue to release high amounts of cortisols; however, the physiology of unresolved PTSD involves a change in how your body processes them. The body adjusts to the chronic release of cortisols by developing an increased number of receptors on the cells that re-uptake these neuro-chemicals. This process interferes with the negative feedback loop that normally sends the message to your brain to stop signaling for more cortisols.
In sum, chronic PTSD is associated with frequent bursts of cortisol and low levels of available cortisol in the bloodstream. This is the physiological explanation of the classic alternation between being overwhelmed and shut-down. It is as if you are driving with one foot on the gas and one on the brakes.
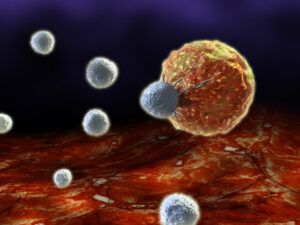
There is an inverse relationship between bloodstream cortisol levels and the immune system. When bloodstream cortisol levels are high the immune system is suppressed. In contrast, when bloodstream cortisol levels are low the immune system is enhanced or “unchecked.” The immune system is associated with inflammation in the body. Such inflammation is necessary when we are fighting off a virus or bacteria. However, when the immune system continues without a target there is a greater likelihood of long-term physical health problems. Research suggests differential health patterns associated with chronic stress and chronic PTSD.
Health problems that are associated with chronic stress in which cortisol is high and immunity is suppressed include:
Health problems that are associated with unresolved PTSD in which bloodstream cortisol is low and immunity is unchecked include:
Let’s take a closer look at the relationship between unresolved trauma and health…

Digestive problems are exceedingly common symptoms associated with PTSD. It is common to feel ashamed or embarrassed. Know you are not alone. When your nervous system is out of balance there is an overproduction of stomach acids and a greater likelihood of digestive conditions such as GERD and IBS. However, there is a way to reclaim a safe and healthy relationship to your parasympathetic nervous system. It is important to reclaim a healthy relationship to your body and to know that relaxation is your friend. Learn about Polyvagal Theory to unlock PTSD.
Normally cortisol rises rapidly after wakening, gradually falls over the day, rises again in the late afternoon, and then falls reaching a low point in the middle of the night. The circadian rhythm is patterned through the cortisol rhythm. With chronic PTSD there is an abnormally flattened circadian cortisol cycle that has been linked to both chronic fatigue syndrome and insomnia.
There are many practices that increase your ability to respond positively to stress and symptoms of PTSD. Here are several practices I recommend:
In my work with clients, I have found that having an understanding of the connections between PTSD and the immune system provides insight into a wide array of auto-immune and medically unexplained symptoms. To be honest, there is no easy, quick fix for the healing of chronic PTSD and related health conditions. This is long-term work; however, as we “unpack” the PTSD suitcase there are gradual improvements in both physical and psychological health. EMDR and somatic psychotherapy are two particularly helpful treatments of choice. In my experience, the greatest success stories for chronic PTSD occur when I am working with team of healthcare professionals that may include your primary care physician, specialists, or alternative health care providers such as acupuncturists or naturopaths.
Dr. Arielle Schwartz is a licensed clinical psychologist, wife, and mother in Boulder, CO. She offers trainings for therapists, maintains a private practice, and has passions for the outdoors, yoga, and writing. She is the developer of Resilience-Informed Therapy which applies research on trauma recovery to form a strength-based, trauma treatment model that includes Eye Movement Desensitization and Reprocessing (EMDR), somatic (body-centered) psychology and time-tested relational psychotherapy. Like Dr. Arielle Schwartz on Facebook or sign up for email updates to stay up to date with all my posts.

Arielle Schwartz, PhD, is a psychologist, internationally sought-out teacher, yoga instructor, and leading voice in the healing of PTSD and complex trauma. She is the author of five books, including The Complex PTSD Workbook, EMDR Therapy and Somatic Psychology, and The Post Traumatic Growth Guidebook.
Dr. Schwartz is an accomplished teacher who guides therapists in the application of EMDR, somatic psychology, parts work therapy, and mindfulness-based interventions for the treatment of trauma and complex PTSD. She guides you through a personal journey of healing in her Sounds True audio program, Trauma Recovery.
She has a depth of understanding, passion, kindness, compassion, joy, and a succinct way of speaking about very complex topics. She is the founder of the Center for Resilience Informed Therapy in Boulder, Colorado where she maintains a private practice providing psychotherapy, supervision, and consultation. Dr. Schwartz believes that that the journey of trauma recovery is an awakening of the spiritual heart.
Beyond Trauma: A Guided Mind-Body Journey of Resilience, Hope and Post-Traumatic Growth